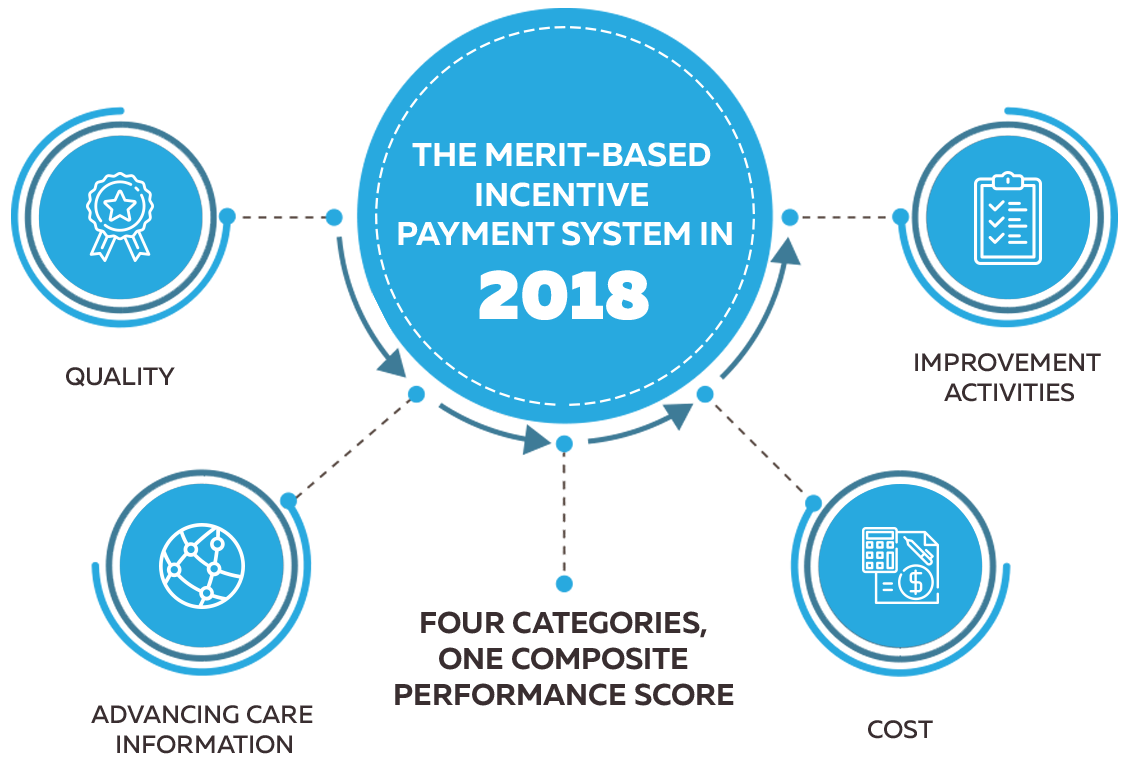
On November 2, 2017, the Centers for Medicare & Medicaid Services (CMS) released updates to the QPP for the 2018 performance period. Follow The Quality Payment Program Year 2. Overview to see major program changes.
In this article we will try to get more details of changes in MIPS performance categories on the 2018 reporting period.
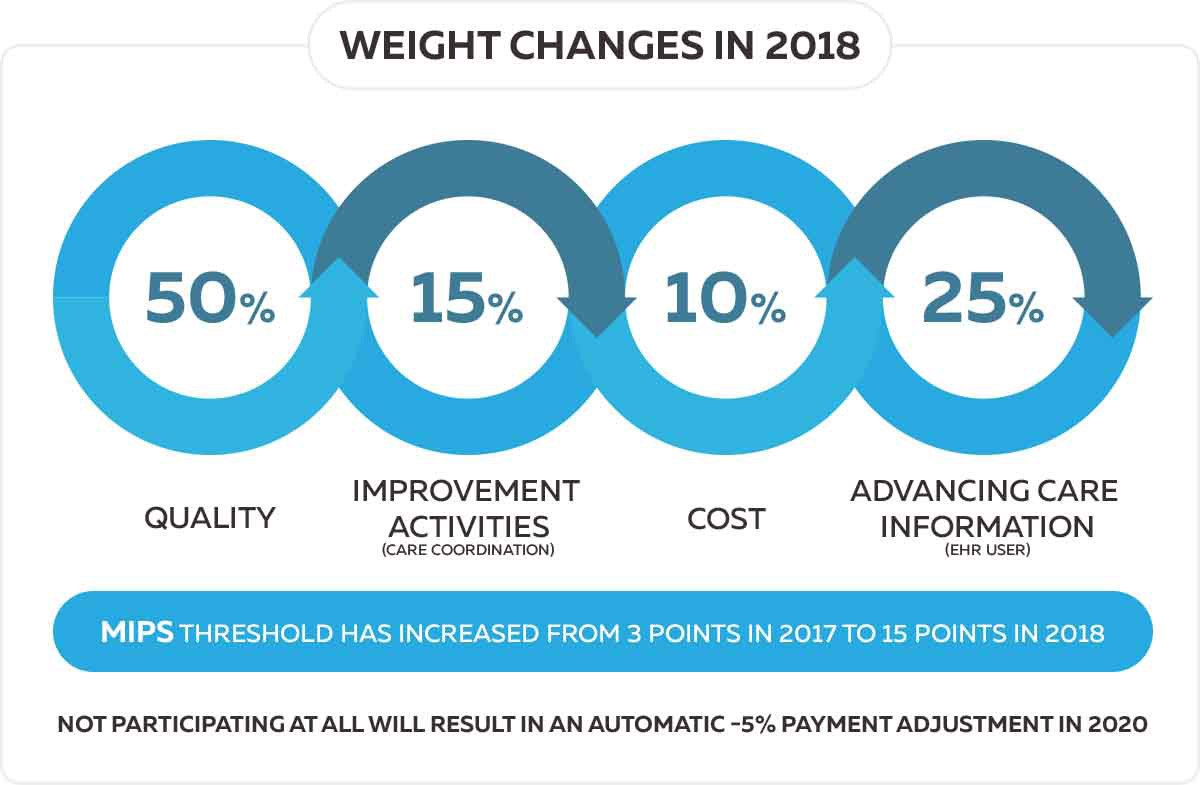
One of the major changes is that CMS set the 2018 MIPS final score threshold at 15 points, up from 3 points in 2017. To avoid the 5% penalty, physicians must earn at least 15 MIPS points.
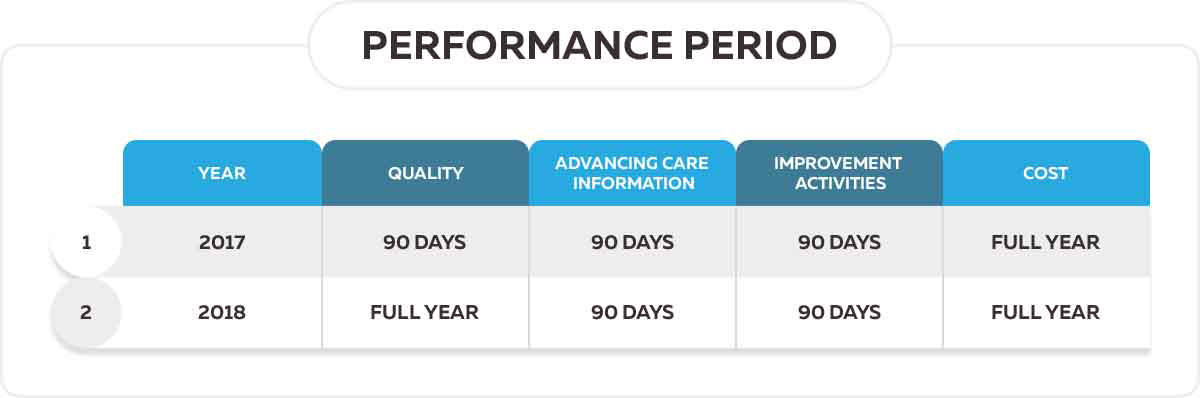
The performance period for the quality and cost categories is a full calendar year (January 1 - December 31, 2018). The performance period for the improvement activities and advancing care information (ACI) categories is any consecutive 90 days.
Final scores above the threshold will receive a positive payment adjustment.
Final scores below the threshold will receive a negative payment adjustment.
ECs in the lowest quartile will receive the maximum payment adjustment for a performance period.
Final scores equal to the threshold will receive a neutral payment adjustment.
MIPS Reporting Options You may report using different mechanisms between categories, but only one method of reporting can be used within each category.
There are some changes in weighting MIPS performance categories. For example, weighting the MIPS Cost performance category to 10% of your total MIPS final score. CMS will calculate cost measure performance; no action is required from clinicians.
| Performance category | Transition Year 1 (2017) | Year 2 (2018) |
|---|---|---|
| Quality | Weight to final score: 60% in 2019 payment year | Weight to final score: 50% in 2020 payment year |
| Cost | Weight to final score: 0% in 2019 payment year | Weight to final score: 10% in 2020 payment year |
| Improvement Activities | Weight to final score: 15% in 2019 payment year | Weight to final score: 15% in 2020 payment year |
| Advancing Care Information | Weight to final score: 25% in 2020 payment year | Weight to final score: 25% in 2020 payment year |
| Performance threshold, Payment adjustment, Performance period | ||
| Performance threshold | 3 points | 15 points |
| Payment adjustment | Ranges from -4% to +4% | Ranges from -5% to +5% |
| Performance period | Minimum 90-day performance period for Quality, Advancing Care Information, and Improvement Activities. | No change for Advancing Care Information, Improvement activities, and Cost performance periods. Minimum 12 month performance period for Quality. |


